Lumbar Microdiscectomy
What is it?
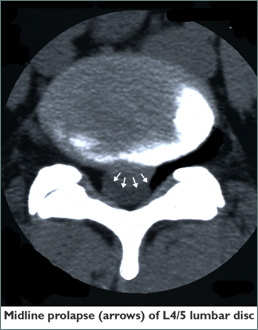
Lumbar microdiscectomy is an operation that involves using microsurgical techniques to access and treat one or more bulging discs in the lumbar spine. By providing magnification and illumination, the operating microscope allows for a limited dissection. Magnifying spectatcles are an alternative used by some surgeons. That portion of the herniated disc which is pinching one or more nerve roots is removed. The term discectomy is derived from the Latin words discus (flat, circular object or plate) and -ectomy (removal).
The operation is commonly offered to patients for relief of leg pain referred from lumbar spine due to herniated disc(s) exerting pressure on roots of the sciatic nerve. It is also offered for other manifestations of pressure on lumbar nerve roots, including weakness (for example an inability to lift the foot at the ankle, termed “foot-drop”) or disturbance in sensation.
The Operation
Incision
The operation is performed with you lying on your stomach. If the operation is viewed through a microscope, this approach only requires a small incision. Your surgeon makes an incision in your lower back. Through this incision, microsurgical instruments are then inserted.
Removal
Once your pinched nerve is located, the extent of the pressure on the nerve can be determined. Using microsurgical techniques, your surgeon removes the herniated portion of the disc as well as any disc fragments that have broken off from the disc. It is also important that the surgeon flushes out the loose stringy material inside the disc, to prevent more of this material coming out (called a “re-prolapse”) in the early post-operative period.
Closure
The operation is completed when your surgeon closes and dresses the incision.
Disadvantages of discectomy
Because the disc is left largely empty within (partly because of the preoperative prolapse of nucleus material, and partly because the surgeon must take away any material likely to prolapse postoperatively) a discectomised disc tends to deflate (that is, lose vertical height) rapidly over the next 3-12 months. There are two unpleasant consequences of this rapid deflation, suffered by approximately 30% of discectomised patients: firstly the facet joints behind the disc become increasingly loaded and may cause increasing low back pain; and secondly deflation of the disc narrows the intervertebral foramen on either side, in which the exiting nerve roots may become compressed. This latter phenomenon is termed “foramenal entrapment”.
Because of these two undesirable sequelae of disc prolapse and discectomy, spinal surgeons often recommend fusion at the time of discectomy: the bone graft or cage used in the fusion operation maintains the height of the disc space and prevents foramenal entrapment and back pain from facet hyperloading.
Recovery
Dr. Brazenor will advise you in general terms about your likely postoperative course, but will stress that your final surgical expectations must come from the surgeon or surgeons to whom he refers you. Dr. Brazenor's pledge is that he will only refer you to surgeons whom he knows are capable of expertly doing the operation you need.
You typically will be up and walking in the hospital by the end of the first or second day after the surgery. You may return to work in 3-6 weeks, depending on how well your body is healing and the type of work/activity level you plan to return to.
